如何看待阿里达摩院研发的新冠肺炎 CT 影像 AI 诊断技术,平均识别不到 20 秒准确率达 96%?
Author: LIN Chumian, Anonymous Zhihu User
Translator: COVID-19 Readings
知乎 (Zhihu) is a popular Quora style question and answer platform in China. This is the question asked on Zhihu about Ali Damo Academy’s COVID-19 AI technology. – the translator
OP (original poster) is a student of radiology. I actually have always worried about the possibility of AI replacing doctors. After all, this is a career that depends on experience, and this is exactly where AI has such an advantage, where it can continously and rapidly learn given current data. With this approach the speed and cost of training a radiologist are both way lower than the current approach, and this “radiologist” even has a great accuracy (reaching 96% according to news).
Meanwhile I’d also like to ask, if (my profession) is to be replaced, how shall I proceed down this career path for the future?
Author: LIN Chumian (Wuhan Union Hospital)
Relevant Occupation: Anesthesiologist at Wuhan Union Hospital, frontline of the COVID-19 epidemic.
In a word: mature medical AI technology that can be put into clinical use is a timely response to the shortage of diagnosis and treatment manpower on the overloaded epidemic frontline.
I signed up for an anesthesia intubation commando and had been in the Union Hospital West Campus for more than a week.
To be honest, the treatment of critically ill patients here on the West Campus that could be described as “tragic and heroic” has left an indelible impression on me.
The rapid deterioration of COVID-19 and the rapid debilitation of severely ill patients are beyond the expectations of many senior clinicians. For example, of the five patients who were intubated the day before yesterday, two had already unfortunately passed…
I clearly remember that they were still conscious before the intubation, and the old pa could still talk to us …

My personal summary is that: severely ill COVID-19 patients have a multi-system, super fast-paced disease; after lung ventilation is damaged, severe hypoxia affects other organs, and SIRS caused by the storm of inflammation can quickly lead to MODS (multiple organ dysfunction syndrome), taking the patients away… So often you can see in the isolation ward that there is a ventilator, hemodialyzer, pump (pressure booster), an infusion rack full of albumin and plasma, and even the big weapon of ECMO – these high-level life support devices, under such circumstances, can only slow down the course of the disease and buy a little time.
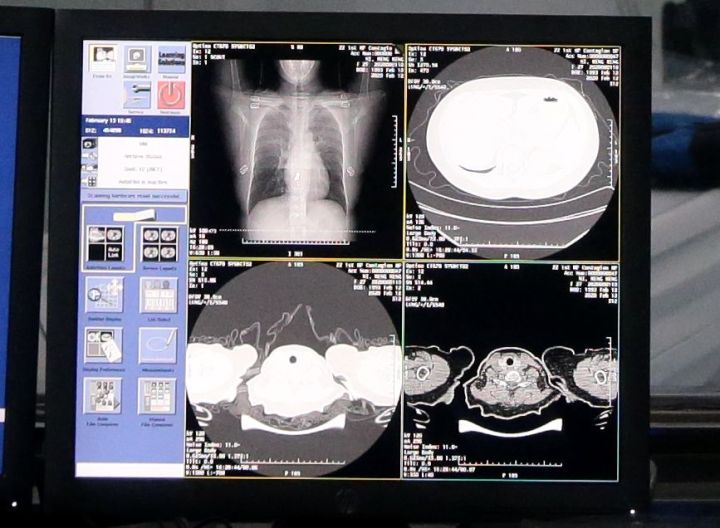
What I deeply realize is that in the treatment of COVID-19, lung CT scan is extremely important! It is no exaggeration to say that lung CT scan is not only an important means for diagnosing viral pneumonia, but also a useful helper for judging the progress of the disease, identifying the turning point, and changing the outcome of the disease! In the above two patients, the recent CT scans of the lungs all demonstrated typical manifestation of COVID-19: white lungs – pointing to very dangerous prognoses.
With 20-20 hindsight, from the perspective of judging the development of the disease, their severe CT scan results were more reliable than the relatively mild clinical manifestations at that time.
Currently, the first-line doctors’ approach to diagnosis and treatment has changed in a pointed way: do CT scans in time, detect the changes early, intubate and get on the ventilator early! Strive to intervene in time before the disease slips from moderate to severe, and interrupt the trend of the disease from becoming more severe through life support treatment. For mild patients, increasing the frequency of CT scans can also help detect potential changes in the disease in time and allow corresponding measures as soon as possible.
Although clinicians would like to give a lung CT scan every two or three days for patients with unclear conditions, the current clinical reality cannot meet this “luxury” demand. In addition to the risks of patient transfer (many patients need to be on oxygen at any given time) and manpower requirements (COVID-19 patients are unlikely to be pushed by their families to do CT scans, instead could only be escorted by medical staff), and the radiation damage of the radiological examination itself, the current imaging capacity on the clinical frontline cannot support high-frequency CT scan needs.
Take my hospital as an example, 800 COVID-19 beds. If three CT scans are performed in a week, it will be 2400 person counts. Plus other clinical examinations, the radiology department will receive an average of 400 persons per day, that is over 100 patients per shift even in 3 shifts. This is a terrifying workload. In addition, the radiology department is also an absolute high incidence area of novel coronavirus infection. Radiologists also need to wear the heavy and hot gears for level III protection when they work. They truly work hard!

What’s most critical is the diagnosis. Clinical matters are important. Radiologists are definitely not done just by casually watching the film. An imaging report directly affects clinical diagnosis and treatment, every single word can have a big impact. The amount of effort involved goes beyond outsiders’ imagination!
In addition, COVID-19 is a “new disease”. The lung images of many mild patients are atypical. For some patients with underlying lung diseases (such as tuberculosis, chronic branch, and COPD), the different diseases have overlapping manifestations, increasing the difficulty of the diagnosis. Generally speaking, there are more than 300 images in a set of CT scans for a COVID-19 patient. Even for senior experts, the time required for reading and diagnosing is at least 10-15 minutes. Most of these are repetitive mechanical labor, which is both effort and time consuming.
At present, in response to the high demand for CT scans, there are two main approaches to solution in clinical practice:

-
Install portable and modular CT equipment (such as “CT container”, a portable CT scanner only for the chest), increase the frequency of CT visits to alleviate CT traffic. Right now, it is common to see imaging / ultrasonic doctors pushing the machine for examination at patients’ bedside.
-
Introduce mature AI image processing diagnostic technology to improve the diagnosis efficiency.
If the diagnostic AI developed by Ali Damo Institute is as claimed, that it can accurately recognize suspected COVID-19 CT scans within 20 seconds, it undoubtedly has great positive significance for the frontline of the epidemic. This means: 1. High CT scan frequency can be satisfied in diagnosis. 2. The work mode of radiologists will change accordingly, from staring at the screen to reviewing and quality assurance of the already classified diagnosis. 3. AI technology will greatly help to balance the diagnostic expertise between different regions, reduce discordant diagnosis rate and misdiagnosis rate. 4. Cloud technology will make remote consultation more convenient.
In addition, returning to the question raised by OP: will AI technology have a huge impact on the employment of radiologists?
In my opinion, it will have an impact, but it will not be significant. In the long run, replacing human labor with AI is a social trend; replacing human labor with computers has increased the overall productivity of society; for industry practitioners, it is an upgrade to be liberated from the repetitive mechanical labor and invested in the formulation of rules and standards and quality assurance of diagnoses, which have more professional value. Of course, this requires future radiologists to know programming and have some IT knowledge, and transform from simply a clinician to a medical-IT inter-discipline talent. But doctors are a career of lifelong learning. This level of challenge should not be a problem for doctors who keep learning.
Looking out of the small framework, technological innovation has never been deterred by individual will. More than 20 years ago, ECG doctors were a very common specialty in China. With the development of technology, automatic ECG identification / reporting technology has eliminated this specialty. Various hospitals may still reserve ECG rooms for physical examinations / inpatients. However, the technology has been generalized and de-specialized. It has become required knowledge for medical students.
Having said all this, to sum it up: whatever that meets clinical needs and helps improve patient outcome is good technology! It is hoped that AI technology can relieve some of the pressure on the COVID-19 frontline and save more lives.
–
Recently, the “Huanggang Experience” on the treatment of NCP shared on the Internet, their view on the importance of lung CT scans coincides with mine.
Author: A Zhihu User
This respondent happened to have studied CT scan + AI from late undergraduate to postgraduate years, therefore volunteering an answer.
There are two statements in the original text that need to be noted. The first is related to data: “The medical AI team of Damo Academy took the latest diagnosis and treatment plan, papers on clinical characteristics of COVID-19 patients published by Zhong Nanshan and other authoritative teams, together with multiple institutions including The First Affiliated Hospital of Zhejiang University, Wanliyun, Changyuanjia and Guppa Hospital, breaking through the limitation of insufficient training data, using CT scan data of more than 5000 cases, learned and trained on sample lesion textures, and developed brand new AI algorithms and models.”
The second is regarding the technical aspect of the AI algorithm: “Alibaba Cloud said that through NLP natural language processing of retrospective data and the use of CNN convolutional neural networks to train the CT scan recognition network, AI can quickly identify the differences between COVID-19 and common viral pneumonia scans, ultimately reaching a recognition accuracy rate of 96%.”
First of all, from the perspective of data, more than 5000 cases is indeed a very large amount of data in the field of CT scan analysis, because each case is a volume of CT images, with each volume containing about 300 slices, so in terms of the sample size of individual images that comes out to 5000 * 300 = 1.5M. This is absolutely a large sample data set even in the field of natural image analysis. It is really not easy to collect such a large amount of data. After all, the number of cases that the respondent could get in years past was only 100+. However, according to the years of experience between the respondent and the doctors, the amount of data is not the key. The key is how much representative and difficult data there is. The doctors are most concerned about the representative and difficult data. A learned as opposed to rule-base algorithm requires a large amount of similar data to learn the correct knowledge, but the amount of difficult case data that doctors are interested in is often small, and our learning algorithms often can only handle the main trend and ignore the difficult cases, but these cases are often the key ones in clinical practice. So for doctors, they are more concerned about whether there are any missing cases in that 4%, and whether there are misdiagnosis in that 96%. Therefore, in the field of medical imaging analysis people do not really focus on accuracy, but instead focus on another criterion, namely TPR (True Positive Rate) + TNR (True Negative Rate). Therefore, I feel that any article that throws out only an accuracy indicator is being sensational. After all, in a medical field with extremely uneven samples, the accuracy measure is pretty “spurious”.
Then it comes to the technical aspect. It should be noted that the algorithm is not simply image analysis, but also includes natural language processing. According to the research experience of the respondent, it is not critical what technology is used. What’s critical is whether the disease really has significant characteristics that can be learned. For example, the task of this algorithm is to identify the images of COVID-19 and common viral pneumonia. Then the clinical radiologists should have their own criteria. This standard will guide developers to try different methods to improve their models, otherwise developers won’t be able to identify problems with the model based on the prediction results. From this point of view, the role of the radiologist is irreplaceable. Another thing that has nothing to do with technology but is important is the granularity of the label. Here comes more than 300 frames of 512 * 512 resolution CT scan data. You only gave me a label of whether or not you have COVID-19. That is way too rough. Doctors are concerned about which frames and which parts are problematic. However, the doctors’ time is precious. According to the respondent’s many years of experience fighting with doctors, it is basically impossible for doctors to give detailed labels of which sections and which parts are abnormal. At present, the existing explanatory methods are basically visualization methods to see which parts have a greater contribution to the probability of disease, but these are learned by the network itself, based only on CT images. But this is not how radiologists work. The radiologists also have to make inferences based on anatomy, medical history, genetics, lifestyle, etc. From this perspective, the role of radiologists is essentially irreplaceable in the near future, not to mention the formulation and implementation of treatment plans and surgical plans.
In short, I feel that the OP should not be intimidated by the 96%. Even if it is 99%, no one would dare use it if it doesn’t solve the problem of true positives and true negatives. Secondly, the respondent can find a medical + AI project for us to collaborate, with you providing detailed image annotations, step by step we can push the development of this field forward, break the data bottleneck from the annotation level, and produce a lot of SCI during this. Wouldn’t that be beautiful :)
Related Articles:
Alibaba’s new AI system can detect coronavirus in seconds with 96% accuracy